Capacity and Consent for MH Treatment and Care
Treatment Criteria and Assessment of Capacity
The treatment criteria for a person are all of the following:- the person has a mental illness
- the person does not have capacity to consent to be treated for the illness (see below), and
- because of the person’s illness, the absence of involuntary treatment, or the absence of continued involuntary treatment, is likely to result in: - imminent serious harm to the person or others, or - the person suffering serious mental or physical deterioration.
For comprehensive information about assessment, reassessment, guidelines and health directives, see Capacity and Decision-Making
Meaning of Capacity to Consent to be Treated
A person has capacity to consent to be treated if the person is capable of understanding, in general terms:- that the person has an illness, or symptoms of an illness, that affects the person’s mental health and wellbeing
- the nature and purpose of the treatment for the illness
- the benefits and risks of the treatment, and alternatives to the treatment, and
- the consequences of not receiving the treatment.
- The person must also be capable of making a decision about the treatment and communicating the decision in some way.
The Act promotes supported decision making by providing that a person may be supported by another person in understanding the matters listed above and in making a decision about treatment. These provisions do not affect the common law in relation to the capacity of a minor to consent to be treated or for a parent of a minor to consent to treatment of the minor.
For judicial discussion about capacity to give informed consent to ECT:
PBU & NJE v Mental Health Tribunal [2018] VSC; 564 [2018] VSC 564; 56 VR 141 PBU & NJE v Mental Health Tribunal [2018] VSC
Analysis of this case:
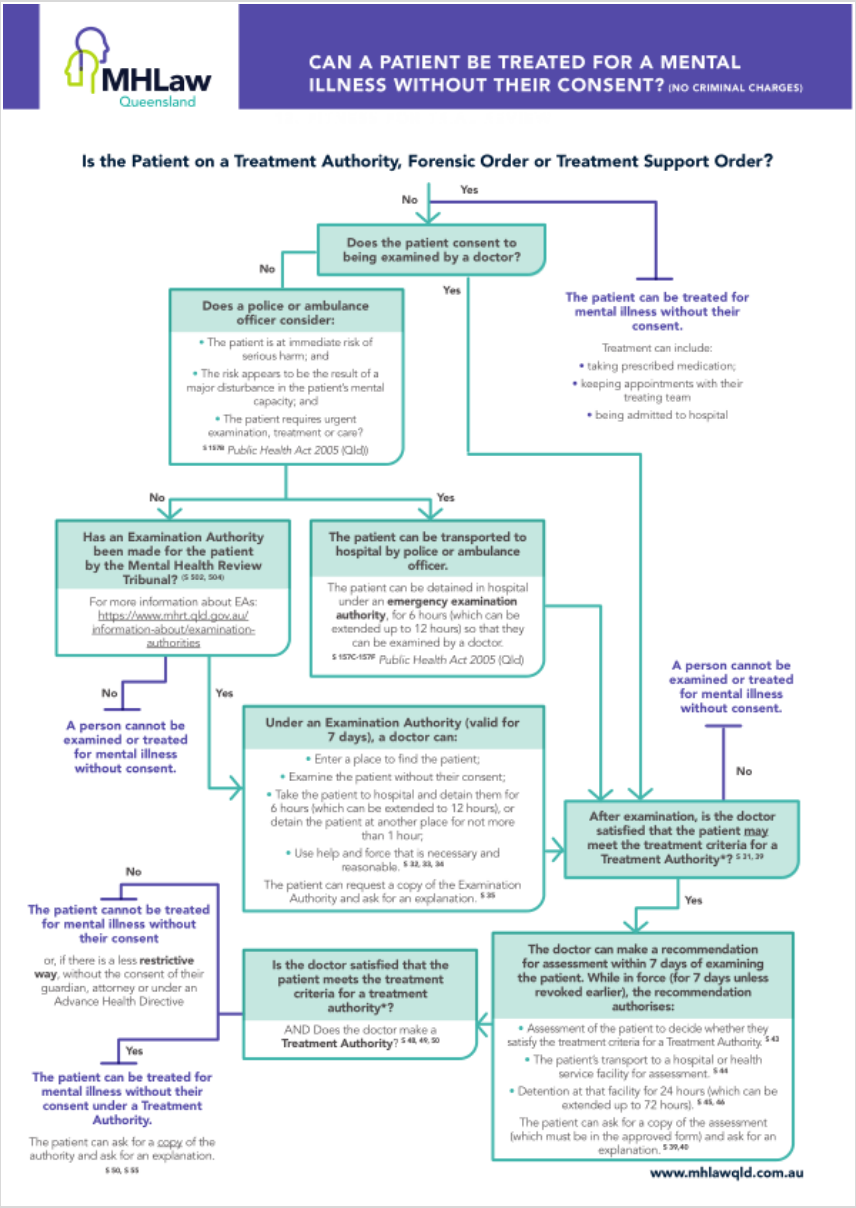
See our Mental Health Act Flowchart for Treatment Consent:
Consent to Treatment Pathways Regarding Healthcare Decisions
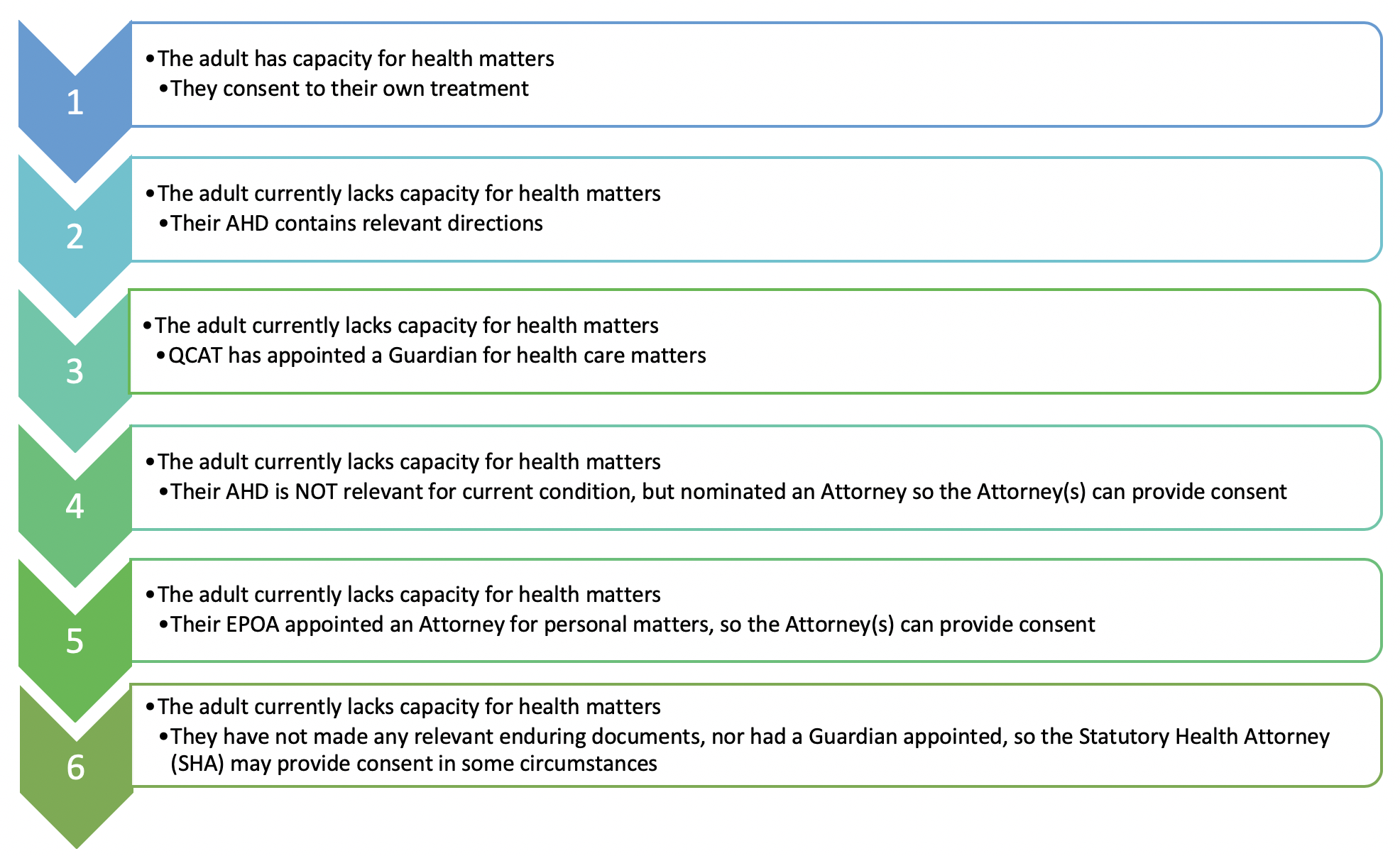
Substitute Decision Makers
Decision makers appointed via AHDs and EPOAs cannot consent to treatment and care that the adult’s AHD explicitly refuses.For more comprehensive information see also Supported Decision Making, Substitute Decision Making and Health Directives
Public Guardian
The Public Guardian, when acting as the appointed decision maker (via AHD/EPOA or QCAT) for adults lacking decision making capacity, enforces decision making guidelines when asked to consent to mental health treatment and care.Where a doctor or authorised mental health practitioner is seeking the consent of the Public Guardian to mental health treatment and care, they must review the Guide: Applying to the Public Guardian for Mental Health Treatment Consent and then complete the Application for Mental Health Treatment and Care Consent Form and submit to:
MHA@publicguardian.qld.gov.au
ph: 1300 653 187
Requests for the Public Guardian’s consent to mental health treatment and care will be considered during general business hours only.
The OPG invites all feedback on the usability of the Application for Mental Health Treatment and Care Consent Form. Please submit any feedback to MHA@publicguardian.qld.gov.au for consideration.
Reference: www.publicguardian.qld.gov.au
Further information is available here: Consent to Mental Health Treatment by the OPG
Framework Consent to Mental Health Treatment by the OPG